What is an Intensive Outpatient Program (IOP)?
An Intensive Outpatient Program (IOP) is a structured and comprehensive form of mental health or substance use treatment that provides more support and therapy than traditional outpatient care but is less intensive than inpatient hospitalization. IOPs are designed to offer individuals a higher level of care while still allowing them to maintain some level of independence and engage in their daily routines.
In an IOP, participants attend therapy sessions three to five days a week and last for several weeks to a few months, depending on the individual’s needs and rate of progress. The duration of IOP programs can vary based on the severity of the mental health condition or substance use disorder, as well as the specific treatment approach used by the program. On average, IOP programs may last from 6 to 12 weeks. Each session may last for a few hours, during which individuals engage in group therapy, individual counseling, psycho-education, and various therapeutic activities. The treatment modalities used in IOPs are evidence-based and tailored to address specific mental health conditions or substance use disorders.
The frequency and intensity of IOP sessions allow participants to work through their challenges, build a strong support network, and practice newly acquired skills in their daily lives. As progress is made, the treatment team may adjust the treatment plan accordingly to ensure that the individual receives the appropriate level of care throughout their recovery journey.
How Do I Know If My Teen Needs an IOP?
If you have a teen who you think may be at risk and could benefit from intensive outpatient care, it is essential to know what to look for. While every teen is different, mental illness generally follows these stages of progression:
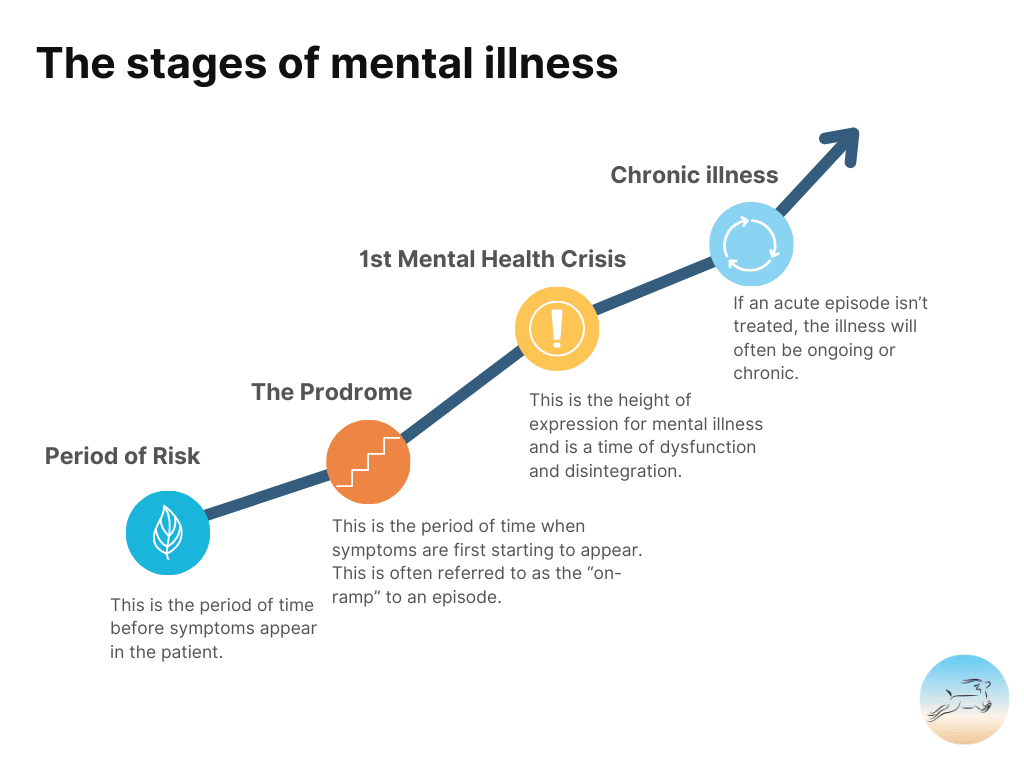
Period of Risk
This is the period of time before symptoms appear in the patient. During this time, especially if mental illness runs in your family, you want to focus on building self-awareness skills, communication skills, and resilience skills with your teenager.
The Prodrome
This is the period of time when symptoms are first starting to appear and is often referred to as the “on-ramp” to an episode. This is where we focus on getting high-quality treatment to patients early on so that we can stop the progression of the illness.
First Acute Episode
An acute episode can look like a psychotic break, a suicide attempt, or a severe depressive episode. This is the height of expression for mental illness and is a time of dysfunction and disintegration. Often, during this time, the client is unable to care for themselves and is at risk of harming themselves and others. Usually, hospitalization or immediate acute care is needed at this stage.
Chronic or Pervasive Mental Illness
If an acute episode isn’t treated, the illness will often be ongoing or chronic and become more challenging to treat. The more prolonged psychosis and mental illness go untreated, typically, the more challenging it becomes to treat it.
Early intervention is essential for teens.
Early intervention for teens is crucial. Mental illness, including substance use disorders, often starts in the teenage years because of how the brain develops. If we can stop the progression of mental illness early on, we can potentially save the teen many years of suffering. Adolescence is a critical period of development that shapes a person’s physical, emotional, and mental well-being for the rest of their lives. During this stage, the brain undergoes significant changes, including the development of executive functions, emotional regulation, and decision-making skills.
Several factors contribute to the importance of early intervention for teens:
- Prevent Progression of Issues: Addressing mental health challenges or behavioral issues early can prevent them from becoming more severe and chronic over time. Early intervention allows for timely identification and treatment, reducing the risk of long-term negative consequences.
- Impact on Academic Performance: Mental health issues can significantly impact a teenager’s academic performance and engagement in school. Early intervention can help teens manage their emotional and psychological well-being, leading to better academic outcomes and opportunities for future success.
- Positive Social Development: Early intervention fosters positive social development by helping teens build healthy relationships, communication skills, and empathy. Addressing behavioral concerns early can prevent social isolation and promote positive peer interactions.
- Preventing Substance Abuse: Early intervention can reduce the risk of substance abuse, as teens may turn to drugs or alcohol as a coping mechanism for untreated mental health issues. Addressing underlying concerns can help prevent the development of harmful coping strategies.
- Family Support: Early intervention involves family engagement, providing parents and caregivers with strategies to support their teens effectively. Strengthening family support can positively influence the teen’s well-being and recovery process.
- Long-Term Outcomes: Addressing mental health challenges early can have positive and lasting effects on a teen’s overall quality of life, mental health, and emotional well-being throughout adulthood.
At each stage of mental illness, programs are able to offer different types of support to effectively treat the client and create pathways to full recovery. The sooner appropriate care is given in mental illness progression, the more likely full recovery is possible. We know that many clients enter into recovery involuntarily during a psychological episode or mental health crisis in a hospital. This is the least desirable path and the least effective entry point for clients to enter into mental health treatment. The earlier a teen is able to receive support, the more successful the support will be.
Common situations in which a teenager might benefit from IOP:
- They’ve recently had a mental health emergency (suicide attempt, overdose, etc.) and need more intensive support while they recover.
- There was a recent change in the family, such as a divorce or a big move.
- The teen is struggling with a new mental health diagnosis, and once-a-week therapy isn’t enough.
- Your teen recently experienced a trauma or overwhelming event, like a car crash, abuse, or a breakup.
- Your teen is struggling, and no one seems to know why. You’ve tried a lot of different things, and nothing seems to be working.
Does my teen need a diagnosis to participate in IOP?
A teenager does not need a diagnosis to be admitted into an Intensive Outpatient Program. However, many teens do come into IOP programs with a diagnosis. IOP tends to be very helpful for the following diagnoses:
- Depression
- Anxiety
- Mood disorders
- ADHD
- Substance use/addiction
- OCD
- Trauma recovery or PTSD
- Self-harm
- Screen Addictions
- Co-occurring disorders
- Bipolar
Tips for families when seeking care:
- First, talk to your teen’s school counselor and pediatrician and ask for their opinion.
- Talk with parents of teens who are doing well and ask them what they might do if their teen were struggling.
- Talk to your teenager and let them know you are worried. Ask them what they think about an IOP program.
- Call us and have us do an initial free assessment.
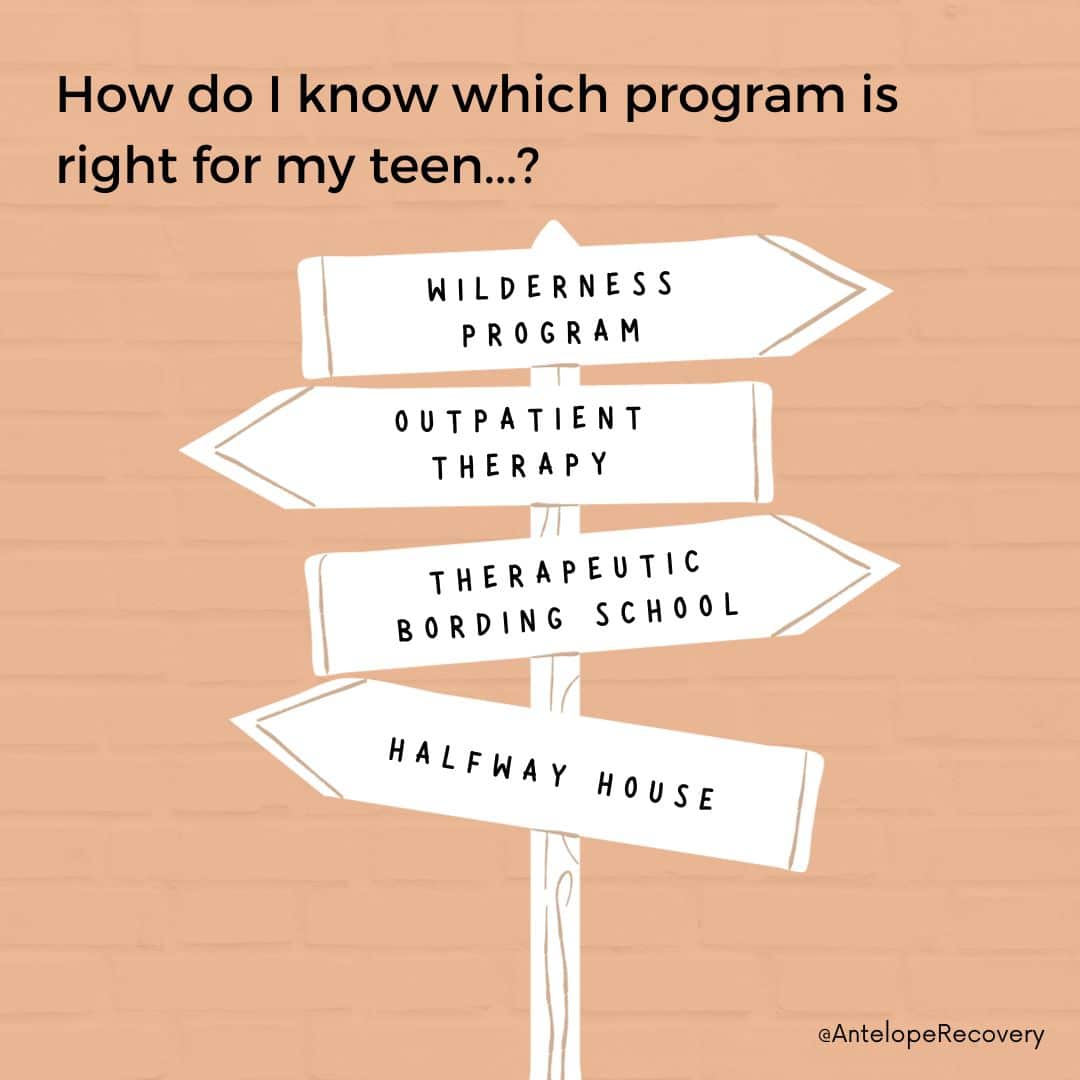
What is the difference between PHP, OP, IOP, and Inpatient Care?
Knowing what type of program is right for your teenager is essential to ensure they receive the appropriate level of care and support for their specific needs. If you’re looking at IOP, OP, and PHP programs and don’t know where to start, begin by seeking a comprehensive assessment from a qualified mental health or addiction professional. This evaluation will help identify the severity of your teen’s condition, the level of care required, and any co-occurring issues. The professional will consider factors such as the intensity of their symptoms, their ability to function in daily life, and the level of family support available when recommending program types. Be sure also to involve your teen in this process.
What is Outpatient Therapy?
Outpatient therapy is a form of mental health treatment that allows individuals to receive a range of therapy and counseling services with flexibility. Outpatient therapy typically is between one to five hours of therapy per week. In outpatient therapy, clients attend regular therapy sessions with licensed mental health professionals, such as psychologists, counselors, or social workers, virtually or at a treatment facility. This flexible approach to therapy is suitable for individuals who do not require intensive, round-the-clock care but still need support and treatment for various mental health conditions, emotional challenges, or behavioral issues. Outpatient therapy provides a safe and confidential space for clients to discuss their concerns, work through problems, and develop coping skills to manage stress, anxiety, depression, or other mental health issues. It can be an essential component of a comprehensive mental health treatment plan, offering support and guidance to individuals seeking to improve their overall well-being.
Scientific Evidence of Effectiveness for Outpatient Therapy:
Numerous studies have shown that outpatient therapy is an effective and evidence-based approach for treating a wide range of mental health conditions. Research consistently demonstrates that psychotherapy provided in outpatient settings can lead to significant improvements in symptoms, increased coping skills, and enhanced overall well-being. Outpatient therapy’s accessibility, cost-effectiveness, and ability to address various mental health concerns have made it a cornerstone of mental health treatment, providing individuals with the support they need to lead fulfilling lives.
What is an IOP?
IOP stands for Intensive Outpatient Program, and it is a level of care that provides more support and structure than traditional outpatient therapy but is less intensive than partial hospitalization or inpatient treatment. Intensive Outpatient Programs are typically between six and twenty hours of support per week. IOP programs are commonly used to treat mental health disorders, substance use disorders, or co-occurring conditions. These programs offer more frequent and intensive therapy sessions, typically three to five days a week while allowing individuals to return home or to a supportive living environment after each session. The main goal of an IOP program is to provide individuals with emergency stabilization support as well as the necessary tools and coping strategies to manage their symptoms, improve functioning, and maintain recovery outside of the treatment setting. IOP programs often include a combination of group therapy, individual counseling, family therapy, and life skills training to address the specific needs of each client. The flexibility and level of care provided by IOP programs make them a valuable option for individuals seeking comprehensive treatment along with the ability to maintain some daily routines and responsibilities.
History of IOP Programs:
Intensive Outpatient Programs (IOP) emerged as a response to the limitations of traditional outpatient care for individuals with mental health disorders and substance use issues. The origins of IOPs can be traced back to the late 1970s and early 1980s, when treatment providers recognized that some individuals required more intensive and structured interventions than weekly outpatient therapy could offer. IOPs gained popularity during the addiction treatment movement of the 1980s and 1990s as a means to address the growing prevalence of substance use disorders. Over the years, IOPs have evolved to become evidence-based, multidisciplinary treatment programs, offering various therapeutic services tailored to the needs of each client. Today, IOPs continue to play a vital role in the continuum of care, providing individuals with a higher level of support while allowing them to continue engaging in their daily lives and responsibilities.
What is a PHP Program?
A PHP program, short for Partial Hospitalization Program, is a structured and intensive form of mental health or substance abuse treatment that falls between inpatient and outpatient care. It is designed for individuals who need more support than traditional outpatient therapy but do not require 24/7 supervision in a hospital setting. In a PHP program, clients attend treatment sessions and therapy five days a week for more than five hours per day. These programs include not only licensed therapists but also licensed medical staff and offer medical and psychiatric support. These programs are more intensive than IOP or OP levels of care.
History of PHP Programs:
The concept of Partial Hospitalization Programs (PHP) can be traced back to the 1950s when there was a growing recognition of the need for alternative mental health treatment options between inpatient hospitalization and traditional outpatient care. PHPs emerged as a response to the overcrowding of psychiatric hospitals and the desire to provide more comprehensive care to patients with severe mental health conditions. The 1963 Community Mental Health Centers Act played a significant role in promoting the development of PHPs by advocating for community-based mental health services. Since then, PHP programs have evolved to incorporate evidence-based therapeutic modalities, offering an array of treatments for mental health disorders and substance use. Today, PHP programs continue to be a valuable resource, providing structured treatment for individuals in need of intensive support while maintaining connections to their communities.
What is Inpatient Treatment?
Inpatient treatment provides around-the-clock support and monitoring, making it the best choice for severely at-risk teenagers. If your doctor recommends inpatient treatment, it typically means that:
- Your teen has received a mental health condition or substance use disorder diagnosis.
- Their symptoms and behaviors are highly disruptive and cause severe harm to themselves or others.
- Their symptoms and behaviors prevent them from participating in daily life.
- They need to leave their daily life in order to stabilize and begin healing.
Depending on your teen’s specific situation, inpatient care may involve residential treatment or psychiatric hospitalization. Psychiatric hospitalization is the most immersive level of care for teenagers. Unlike residential treatment centers, hospitalization is for teens in immediate crisis.
If your teenager is actively suicidal, displays violence or aggression, or engages in dangerous behavior, we will usually suggest hospitalization. Hospitalization can provide a supportive environment with care from licensed clinicians. When your teen is safe and stable, your treatment team may recommend therapy, partial hospitalization, or detoxification (for substance use dependence).
What questions to ask programs if you’re considering signing your teen up for IOP:
When considering enrolling your teen in an Intensive Outpatient Program (IOP), we recommend asking these questions when researching programs. This will help you to make an informed decision about their care.
Here are some critical questions to ask IOP programs before signing up your teen:
- What is the program’s treatment approach, and what modalities do they use?
- Will the team provide the parents with regular updates? How does communication between the clinical team and the parents work?
- What if my teen does not want to participate? How will the program handle that?
- What are the qualifications and credentials of the treatment team?
- What is the duration of the program, and how many sessions are held each week?
- What are the program’s hours of operation?
- What types of mental health or substance use disorders does the program specialize in treating?
- How does the program assess and tailor treatment plans to meet individual needs?
- Does the program involve family therapy or family involvement in the treatment process?
- What are the program’s success rates or outcomes?
- How is confidentiality and privacy ensured for participants?
- Are there any additional support services or resources offered outside of therapy sessions?
- Does the program work with insurance providers or offer financial assistance options?
- How does the program support participants transitioning back into daily life after treatment?
- What is the approach to relapse prevention and aftercare planning?
- Can the program provide testimonials or references from former participants or their families?
Three red flags you should watch out for when choosing an IOP program:

Despite there being so many regulations and protections from the state, insurance companies, and accreditation services that are designed to assure the quality of care, there are still important red flags to look out for when choosing an IOP program. The last thing you want to do is invest a lot of time and money into your teenager’s well-being and then be met with poor service due to burnt-out workers who are underpaid and just cannot give your family the attention you need or poor business practices.
Here are three red flags to look out for when choosing an IOP program:
1. Unrealistic Promises or Guarantees: Be cautious of IOP programs that make unrealistic promises or guarantees about treatment outcomes or rapid progress. Recovery is a complex and individualized journey, and no program can guarantee specific results. Reputable IOPs provide realistic expectations and focus on supporting participants throughout their recovery process, acknowledging that progress may vary for each individual. There is, unfortunately, no magic pill for recovery. Good programs will embrace that fact and be honest with you about what that means for your child.
2. Lack of Family Involvement or Support: Family involvement is essential in the treatment of adolescents and teenagers. Red flags may include IOP programs that do not encourage or include family therapy sessions or support for family members. A quality program will recognize the significance of the family’s role in the recovery process and provide assistance to caregivers.
3. Poor Communication or Transparency: Pay attention to how the IOP communicates with you during the admissions process. Red flags include a lack of clear communication, difficulty reaching staff, or evasiveness when answering your questions. A reputable IOP should be transparent about its treatment approach, privacy policies, costs and be responsive to your inquiries. If a program is hard to get in touch with in the beginning or is not transparent about its approach to specific diagnoses, you should avoid working with them.
What is the difference between adult IOP and teen IOP?
The main difference between Adult Intensive Outpatient Programs (IOP) and Teen Intensive Outpatient Programs lies in the treatment approach, therapeutic focus, and unique needs of each age group.
Treatment Approach: Teen IOPs are tailored to meet the unique needs of adolescents. These include issues related to school and academic stress, peer relationships, family dynamics, and challenges associated with early-onset mental health conditions. Teen programs tend to be less education-heavy and far more focused on connection-building, developing communication skills, and exposure to long-term coping skills and hobbies. Teen programs are more about planting seeds and creating safety. On the other hand, Adult IOPs are designed to address the specific mental health concerns and challenges faced by adults, such as later-stage mental illness and addiction symptoms that come after decades of living with these struggles. Adult programs also discuss adult issues such as financial struggles, marriages, and work-related issues. Adult treatment approaches tend to emphasize education, financial and housing stabilization, as well as individual therapy.
Family Involvement: While family involvement is essential in both Adult and Teen IOPs, Teen IOPs place more emphasis on family therapy and engagement. Teen programs recognize the significant role parents and caregivers play in the recovery process of adolescents.
Education and School Support: Teen IOPs often integrate educational support to help teens maintain their academic progress during treatment. Programs may collaborate with schools to ensure teenagers’ educational needs are met while attending the IOP.
8 Reasons why a virtual IOP could be the best fit for your Teen
Virtual Intensive Outpatient Programs (IOPs) have emerged as an innovative and accessible option for adolescents and teenagers seeking mental health or substance use treatment. Virtual IOPs have been around for over 15 years; however, during the COVID-19 pandemic, the popularity of this intervention skyrocketed. Online IOPs utilize digital platforms to deliver therapeutic support, offering numerous benefits that might make them the best fit for your teenager’s needs.
Here are 8 reasons why a virtual IOP could be the ideal choice:
- Flexible Schedule: Virtual IOPs can work with a busy teenager’s schedule, allowing them to continue with school, sports, and other obligations and commitments while attending treatment.
- No drive time: Virtual care can work really well for families where all caregivers work and cannot drive a teen to treatment after school, for divorced families or more complex family structures where driving the teen to treatment would be a barrier to care. Regardless of geographic location, your teen can access the help they need.
- Privacy and Confidentiality: Your teen is unlikely to run into a peer they know from school, sports, or other local areas in a virtual IOP. Because clients come from all over the state, there is more privacy and confidentiality for your teen.
- Specialized staff: Because a virtual IOP is not location-bound, programs hire specialists from all over the country to support your child.
- Family Involvement: It can be easier for the family to be involved in care when care is virtual. You can video call into therapy sessions and trust that you can still show up for your teenager, even if you are away from home or have a demanding schedule.
- Continuous Care: Virtual IOPs reduce the risk of treatment gaps or disruptions.
- Comfort and Familiarity: Teens often feel more relaxed and open in their home environment during therapy sessions.
- Embedded care: Because treatment is virtual, care is integrated directly into the teenager’s life. Because of this, virtual IOP can be a good fit for a teen who needs to make changes directly at home or school.
Virtual IOPs blend convenience, technology, and evidence-based therapy to create an engaging and practical treatment experience for your teenager. Consider exploring this modern approach to support your teen’s journey toward healing, growth, and long-term well-being.
IOP can work for your family
Choosing the best intensive outpatient program for your teen is a significant decision, and we understand the importance of finding the right fit for your family. At Antelope Recovery, we take pride in offering a wide range of intensive outpatient programming options tailored to meet the unique needs of adolescents and their families. Our dedicated team of professionals is committed to providing comprehensive care and support every step of the way. Whether it’s addressing substance abuse, mental health issues, or other challenges, we’re here to help your teen thrive. If you’re seeking a trusted partner in your teen’s journey towards recovery, look no further than Antelope Recovery. Contact us today at (303) 578-2391 to learn more about our services and how we can assist your family in achieving lasting positive change. Or, schedule a consultation for treatment here.